A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of conditions beginning with that letter.
Click 'Topic Index' to return to the index for the current topic.
Click 'Library Index' to return to the listing of all topics.
Boxer’s Fracture
A boxer’s fracture is a break in a bone at the outer edge of the hand. The bone is under the pinky finger bones. Boxer’s fracture gets its name because it is often caused by punching a hard surface with the fist.
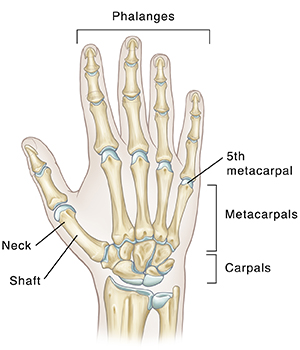
Understanding the bones of the hand
The bones of your hand are called metacarpal bones. They connect the bones of your fingers (phalanges) to the bones of your wrist (carpals). The fifth metacarpal is the metacarpal of the fifth finger (pinky). A metacarpal bone has a long section of the bone (shaft) connected to the end of the bone. The area where the shaft connects to the end of the bone is called the neck. The neck is the weakest point of the bone. This is where a boxer’s fracture happens.
What causes boxer’s fracture?
You may have a boxer’s fracture from an injury. This most often happens from punching a hard object, such as a punching bag, wall, or other firm surface. You may also get a boxer’s fracture if you fall on your closed fist.
Symptoms of boxer’s fracture
Symptoms of a boxer’s fracture can include:
-
Painful bruising and swelling of the hand
-
Bent, claw-like pinky finger that is out of its normal position
-
Limited range of motion of the ring (fourth) and pinky fingers
-
Change in the shape of the knuckle
Diagnosing boxer’s fracture
Your healthcare provider will ask about your symptoms and about how you injured the hand. They will also examine your hand. You may have an X-ray of the hand. This uses a small amount of radiation to create an image of the bones.
Treatment for boxer’s fracture
Your healthcare provider may refer you to an orthopedist. This is a healthcare provider who specializes in treating bone, muscle, joint, and tendon problems. Your treatment may first include:
-
Cleaning any cuts
-
A tetanus vaccine, if you have cuts
-
Resting your hand and keeping it raised (elevated) as much as possible for a few days
-
Putting ice on it throughout the day
-
Taking prescription or over-the-counter pain medicine
-
Wearing a splint for several weeks
You may need to have your bones put back into position. You may have a local pain medicine to keep you from feeling pain during this process. Your healthcare provider will then move the bones back into place.
Surgery for boxer’s fracture
You may need surgery. This is done by an orthopedic surgeon. The surgeon makes a cut in the skin to put your bones back into place. You may need surgery if:
-
The bone has broken through the skin
-
The bone is broken in several places, or is significantly out of place or bent
-
You use your hands and fingers for your work. For example, if you are a musician, craftsman, or seamstress.
-
Your hand doesn’t heal normally
After surgery, you may have physical therapy to help you heal. The therapy includes treatments and exercises.
What happens if you don’t get treated?
An untreated boxer’s fracture can cause problems such as:
-
You may be less able to grip objects.
-
You may not be able to move your hand or finger as much as you did before the injury.
-
Your finger may not look normal.
Preventing boxer’s fracture
If you box, make sure you use the correct method and equipment.
How to manage boxer’s fracture
Your healthcare provider may tell you to:
-
Keep your splint from getting wet.
-
Keep your bones strong and help your fracture heal. Eat foods with vitamin D, calcium, and protein.
-
Stop smoking. If you smoke, your fracture may not heal as quickly or correctly.
-
Be careful while your hand heals. You may need to use a brace for a while.
When to call the healthcare provider
Call your healthcare provider right away if any of the following occur:
-
Numbness or tingling in your fingers
-
Fingers that look blue
-
Pain or swelling that gets worse
-
Problems with your splint
-
Skin in the area is red, painful, or swollen
Online Medical Reviewer:
Raymond Turley Jr PA-C
Online Medical Reviewer:
Stacey Wojcik MBA BSN RN
Online Medical Reviewer:
Thomas N Joseph MD
Date Last Reviewed:
6/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.