Having Cardiac Resynchronization Therapy (CRT)
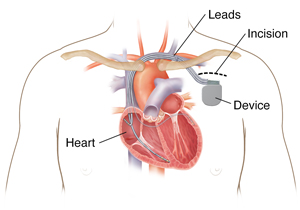
Your healthcare provider advises that you have cardiac resynchronization therapy (CRT). This is a procedure to place a small device (biventricular pacemaker) in your chest. The device has wires that can pace both the left and right ventricles (bottom chambers) of the heart. When people have heart failure and electrical conduction diseases such as bundle branch blocks, the right and left sides of the heart contract at different times (called dyssynchrony). This can cause a weakening of the heart and less efficient blood flow. CRT improves the timing of your heart’s contractions. This makes sure that both sides of your heart contract at the same moment (called resynchronization). This helps your heart pump better to get blood and oxygen to the rest of your body.
Depending on your condition, you may have a combined device. This means a biventricular pacemaker and an implantable cardioverter-defibrillator (ICD). An ICD can treat very fast heart rhythm problems. Biventricular pacemakers with defibrillator are called cardiac resynchronization therapy defibrillators (CRT-D). Your healthcare provider will decide which device is better for you.
Talk with your healthcare provider about any questions or concerns you have before the procedure. The procedure takes about 1 to 3 hours. You will generally stay in the hospital overnight. This is to make sure the device is working correctly and to check your incision. Most people return to their normal routine a few weeks after the procedure. Here’s what to expect before, during, and after the procedure.
Before the procedure
Before your procedure, you may have certain tests to make sure CRT is right for you. You may have a cardiac catheterization, an electrocardiogram (ECG), and a stress test using electrocardiogram. You may also have an echocardiogram (echo). These tests tell your healthcare provider about how well your heart is working.
You may need to stop taking certain medicines for a few days before the procedure. This includes medicines that thin your blood. If you take medicines for diabetes, you may need to change your dose before and after the procedure or even stop some altogether. Talk with your provider for specific instructions.
You will not be able to eat or drink a certain number of hours before surgery. Follow your provider's instructions. If you take medicines in the morning, ask your provider if you can take them with a sip of water.
Let your healthcare provider know about:
-
All prescription medicines you take
-
All over-the-counter medicines you take, such as aspirin
-
All herbs, vitamins, or other supplements you take
-
Any allergies you have
-
Any history of kidney disease
-
Any recent symptoms of colds or infections
-
Any past problems with anesthesia
-
Pregnancy or suspected pregnancy
During the procedure
You’ll be sedated during the procedure using pain medicine and sedatives. General anesthesia is rarely used. During the procedure:
-
You will lie down on an X-ray table in a special lab. An IV (intravenous) line will be put in your arm or hand. This is a thin, flexible tube. It lets your healthcare provider give you medicines to help you relax and to prevent pain.
-
Monitors and sensors are put on your body to check your heart, blood pressure, and blood oxygen level.
-
The area where the device is being inserted will be shaved, if needed, and cleaned with antiseptic solution.
-
A numbing medicine (local anesthetic) is injected into your chest below your collarbone.
-
Your healthcare provider will make an incision about 2 inches long in the skin of your chest.
-
The healthcare provider then puts the device wires (leads) into a large vein that sends blood to your heart. The wires are guided into your heart. Special live X-rays (fluoroscopy) are taken to make sure the leads are in the right place on both sides of the heart.
-
The leads are then tested to be sure everything is connected and working correctly. This may feel as if your heart is racing.
-
If the leads are in the correct place and working, they are attached to the CRT device (pacemaker or defibrillator). The device is put through the incision and placed under your skin.
-
Your healthcare provider will then close the incision with stitches, staples, or surgical glue. They may apply a dressing.
After the procedure
You'll go to the recovery area, where you'll stay until the sedative medicine wears off. A healthcare provider will give you pain medicine as needed. You may need to stay in the hospital overnight. This is so your provider can check and adjust the settings on your CRT device and monitor your incision site. After you leave the hospital, follow all of your provider's advice. They'll give you specific instructions on how to care for your incision. You'll also need to limit how you move your arms for a certain period of time. Your provider will monitor your CRT device at regular intervals to make sure the device is working correctly and to check battery usage. It's important that you keep all follow-up appointments.