A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of medical procedures beginning with that letter.
Click 'Back to Intro' to return to the beginning of this section.
Discharge Instructions: When Your Baby Cries
The way your baby cries can tell you how they are feeling. It can also alert you to the baby’s needs. This sheet will help you understand what it means when your baby cries and what you can do to help.
Crying
It’s normal for babies to cry. Sometimes the baby just wants to be held. But if the crying doesn’t stop, look for a cause. Common causes of crying include:
-
Hunger.
-
Discomfort, such as a wet diaper, clothes that are too tight, feeling too hot or too cold, or gas pains.
-
A stuffy nose. This can make it hard for the baby to breathe.
-
Stress or overstimulation.
-
Illness.
What to do when your baby cries
Crying can be the baby’s way of telling you there’s a problem. The baby trusts you to respond to crying and fix whatever is causing the problem. You already know your baby better than anyone else, although figuring out exactly what your baby is telling you may take some guesswork at first. If holding the baby doesn’t help, here are some other things you can try:
-
Try feeding, in case your baby is hungry. To help prevent gas pains, burp the baby about every 5 minutes while feeding. Keep the baby’s head higher than the rest of the body while feeding. Don't overfeed your baby. This can cause discomfort. Try to wait at least 2 hours in between feedings.
-
Check the baby’s diaper. Change it if needed.
-
Give your baby a warm bath. Or hold a damp, warm towel on the baby’s stomach for a little while. This may calm some babies.
-
Rock or walk with your baby. Motion is soothing. Some parents and babies enjoy using slings or other hands-free baby carriers for this purpose.
-
Offer your baby a pacifier at naptime or bedtime. Don't attach a string or clip to the pacifier. And don't give the pacifier until you have fully established breastfeeding. Breastfeeding and regular checkups help lower the risk for sudden infant death syndrome (SIDS).
-
Wrap the baby snugly in a blanket. This is called swaddling. It may help the baby feel safe and secure. (See the box later in this sheet to learn how to swaddle your baby.) Swaddling is common throughout the world but has become controversial. Swaddling can make a baby too hot. More importantly, if the blanket becomes loose or a swaddled baby rolls over, the baby can suffocate. Discuss swaddling your baby with your baby's health care provider.
-
Hold your baby against your bare chest. Skin-to-skin contact can be comforting to the baby.
-
Never shake your baby. Babies who are shaken can suffer lifelong disabilities. If you can't calm your baby, it is OK to put them in a safe place and take a short break. Also ask a family member or friend to give you a break from your baby.
-
If the baby has a stuffy nose, use a bulb syringe to clear it. Your baby’s provider can show you how to do this.
-
Check for signs of illness, such as fever or diarrhea. If the baby seems sick, contact the provider.
When to contact your child's health care provider
Contact the provider if your baby:
-
Has diarrhea or vomiting, or is feeding poorly.
-
Has a fever (see Fever and children, below).
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The health care provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the provider what type to use instead. When you talk with any provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Contact the health care provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° F (38° C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older
How to swaddle your baby
Wrapping your newborn baby securely in a lightweight blanket (swaddling) may help your baby feel warm and safe. But swaddling may have some risks and needs to be done safely. Don't swaddle babies older than 2 months, because they are old enough to learn other ways to comfort themselves. They are also starting to try to roll onto their side or stomach. Here is one method of swaddling:
-
Fold a square blanket diagonally to make a triangle. Turn the triangle so the flat base is at the top and the point is at the bottom.
-
Lay the baby on top of the blanket with the head over the straight base of the triangle and the feet toward the point.
-
Pull one side of the triangle all the way over the baby’s torso and tuck it under the baby’s body. A baby is most comfortable with the arms folded over the chest. It is best to leave one arm free so the baby can suck on their fingers and gradually learn to calm themself without needing to be swaddled.
-
Bring the bottom of the blanket loosely over the baby’s feet and all the way up to the neck. It's very important to keep the baby's feet and legs free to move. Your baby's legs should be able to bend up and out at the hips. Don’t place your baby’s legs so that they are held together and straight down. This raises the risk that the hip joints won’t grow and develop correctly. This can cause a problem called hip dysplasia and dislocation. If your baby has hip dysplasia, don't swaddle.
-
Wrap the other side of the triangle across the baby’s chest.
-
After your baby is swaddled, check often for the following:
-
The blanket stays secure. A loose blanket can cover the baby’s face and cause suffocation. But tight blankets may make it hard for babies to breathe, so be sure you can easily insert three fingers between the blanket and the baby's chest.
-
The baby is lying on their back. Babies lying on their sides or stomachs (or babies who roll onto their sides or stomachs) have a higher risk of SIDS.
-
The baby is not overheated. This may increase the risk for SIDS. Try to use lightweight blankets or sheets for swaddling.
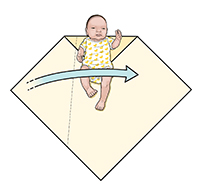 |
| Figure 1. |
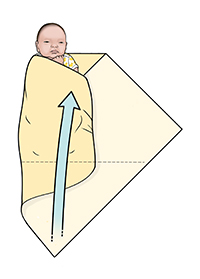 |
| Figure 2. |
 |
| Figure 3. |
Online Medical Reviewer:
Daphne Pierce-Smith RN MSN
Online Medical Reviewer:
Raymond Turley Jr PA-C
Online Medical Reviewer:
Shaziya Allarakha MD
Date Last Reviewed:
2/1/2025
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.