A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of medical procedures beginning with that letter.
Click 'Back to Intro' to return to the beginning of this section.
Treatment for Your Child’s Aortic Stenosis (AS)
Your child has aortic stenosis (AS). This condition occurs when the aortic valve doesn’t open all the way. It can also occur when the area above or below the valve is too narrow. As a result, blood flow from the heart to the rest of the body (except the lungs) is blocked. Children with severe or critical AS need immediate treatment. Treatment choices include balloon valvuloplasty, aortic valve repair, or aortic valve replacement.
Your child’s experience with balloon valvuloplasty
Balloon valvuloplasty is a heart procedure using a thin, flexible tube called a catheter. A cardiologist who has special training to use these catheters to treat heart problems (cardiac catheterization) does this procedure. It lasts about 2 to 4 hours and takes place in a catheterization lab at the hospital. You’ll stay in the waiting room during the procedure.
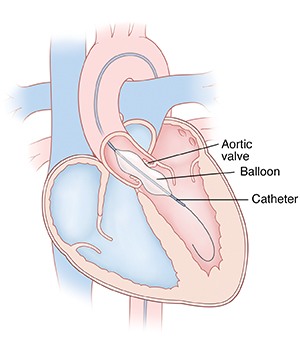 |
| A balloon on a catheter is inflated to open the stenotic (narrowed) aortic valve. |
-
Before the procedure. You’ll be told to keep your child from eating or drinking anything for a certain amount of time before the procedure. Follow these instructions carefully.
-
During the procedure. The healthcare provider inflates a balloon on the tip of the catheter to open the stenotic (narrowed) aortic valve. Your child is given medicine (sedative or anesthesia). This is to help them relax and not feel discomfort or pain during the procedure. A breathing tube may be placed in your child’s trachea (windpipe) during this time. Special equipment monitors your child’s heart rate, blood pressure, and oxygen levels. The catheter insertion site (the groin) is cleaned and numbed. Then the catheter is inserted into a blood vessel in the groin. With the help of live X-rays, the catheter is guided up through this blood vessel into the heart. Your provider may inject contrast dye through the catheter. The dye allows the inside of the heart to be seen on X-rays. The provider will inflate a small balloon at the end of the catheter 1 or more times within the aortic valve. This forces the valve leaflets to open. Then they will remove the catheter and balloon.
-
After the procedure. Your child is taken to a recovery room. You can stay with your child during much of this time. It may take several hours for medicines to wear off. Pressure is applied to the catheter insertion site to limit bleeding. The provider will tell you how long your child needs to lie down and keep the insertion site still. Your child is cared for and monitored until they can leave the hospital. An overnight hospital stay is often needed.
Risks and complications of balloon valvuloplasty
The risks and complications include the following:
-
Reaction to contrast dye
-
Reaction to sedative or anesthesia
-
Pain, swelling, redness, bleeding, or drainage at the catheter insertion site
-
Leakage of blood through the aortic valve back into the left ventricle (valve insufficiency)
-
Abnormal heart rhythm (arrhythmia)
-
The need for further treatment to repair or replace the valve
-
Injury to the heart or a blood vessel
Your child’s experience with valve repair or replacement
Valve repair or replacement is done with open heart surgery. A pediatric heart surgeon does the heart surgery. The surgery lasts about 4 to 6 hours. It takes place in an operating room in a hospital. You’ll stay in the waiting room during your child’s surgery.
-
Before surgery. You’ll be told to keep your child from eating or drinking anything for a certain amount of time before surgery. Follow these instructions carefully.
-
During surgery. Your child is given medicine (sedative and anesthesia) to sleep and not feel pain during surgery. A breathing tube is placed in your child’s trachea (windpipe) during this time. Special equipment monitors your child’s heart rate, blood pressure, and oxygen levels. Your child is also placed on a heart-lung bypass machine. This allows blood to continue flowing to the body while the heart is stopped so that it can be operated on. Your surgeon will make an incision in the chest through the sternum (breastbone) to access the heart.
-
With valve repair, the surgeon opens the aortic valve by cutting through thickened or fused leaflet tissue. A patch can also be used to make the valve larger, if needed.
-
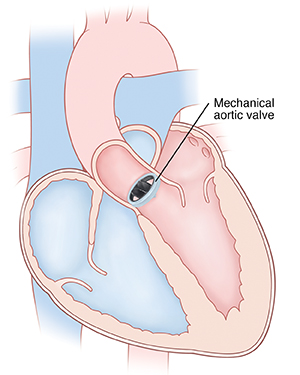
With valve replacement, the surgeon replaces the aortic valve with an artificial one that is either biological or mechanical. Biological valves are made from human or animal tissue. Mechanical valves are made from material such as ceramic or metal. Or, the child's own pulmonary valve may be removed and used to replace the aortic valve. This is known as the Ross procedure, which can be especially beneficial as the valve grows with your child. The pulmonary valve is then replaced with a valve from a human donor (homograft).
-
After surgery. Your child is taken to a critical care unit to be cared for and monitored. You can stay with your child during much of this time. They will stay in the hospital for at least 5 to 7 days. When your child is ready to leave the hospital, you’ll be given instructions for home care and follow-up.
Risks and complications of heart surgery
Risks and complications may include the following:
-
Reaction to sedative or anesthesia
-
Leakage of blood through the aortic valve back into the left ventricle (valve insufficiency)
-
Abnormal heart rhythm (arrhythmia)
-
Infection
-
Bleeding
-
Nervous system problems, such as seizure or stroke
-
Abnormal buildup of fluid around the heart and lungs
-
Death
When to call your child's healthcare provider
After the balloon valvuloplasty procedure or heart surgery, call your child's healthcare provider right away if your child has:
-
Increased pain, swelling, redness, bleeding, or drainage of an incision or insertion site
-
A fever (see "Fever and children" below). Ask the provider about target temperatures for your child.
-
Chest pain
-
Increased tiredness
-
Trouble breathing
-
Prolonged nausea or vomiting
-
A cough that won’t go away
-
An irregular heartbeat
-
Passing out
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years old, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° (38°C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older
Online Medical Reviewer:
Pat F Bass MD MPH
Online Medical Reviewer:
Scott Aydin MD
Online Medical Reviewer:
Stacey Wojcik MBA BSN RN
Date Last Reviewed:
3/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.